 Instructions for reducing the resistance of microbes to existing antibiotics are given by the World Health Organization with new list of the most important resistant microbes in the world
Instructions for reducing the resistance of microbes to existing antibiotics are given by the World Health Organization with new list of the most important resistant microbes in the world
Five more germs that cause resistant infections have been added to the World Health Organization's (WHO) list of dangerous bacteria, as their frequency has increased in the global population. The mortality they cause ranges between 11-30% and is not expected to decrease anytime soon since there are no drugs to treat them.
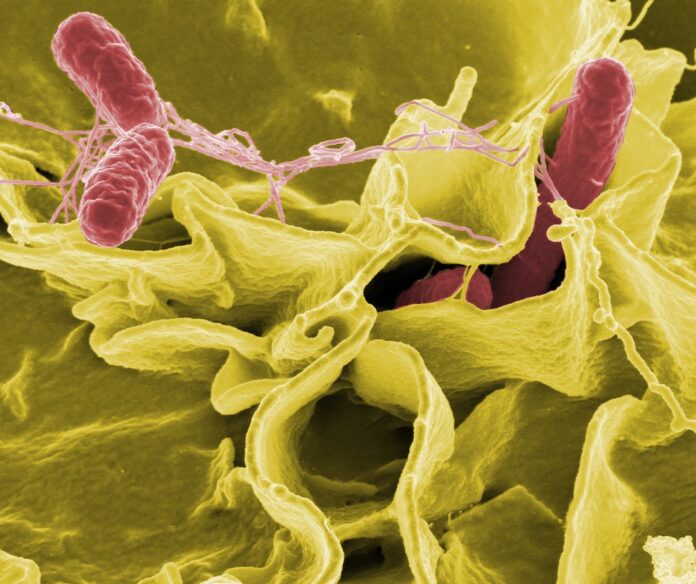
Salmonella, Shigella, Neisseria gonorrhoeae, Pseudomonas and Staphylococcus aureus are well-known bacteria, but this year they enter the WHO's list of dangerous microbes, while the rifampicin-resistant tuberculosis bacterium creates a separate category by itself, showing the increasing the risk of resistant tuberculosis.
Accordingly, depending on the region of the world, there is also an increase in other bacteria that are not included in the list, because their frequency is limited to these places and not internationally.
 The list of new critical, high and medium priority bacteria
The list of new critical, high and medium priority bacteria
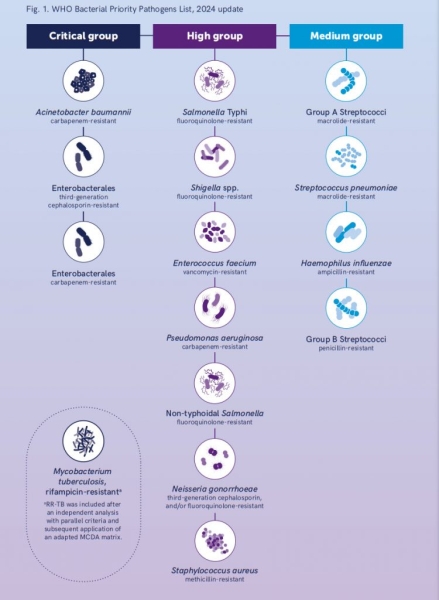
In the new updated WHO list of Priority Pathogenic Bacteria 2024, 24 pathogenic microbes are included, belonging to 15 families of bacteria resistant to existing antibiotics. These microbes are grouped into three categories, critical, high and medium priority, depending on their effects, with the first criterion being mortality, which for the critical category exceeds 30%, for the high priority it ranges between 20-30% and for the average priority varies between 11-20%.
In addition, the frequency for critical priority is more than 10,000 cases per million population, high between 5001-10,000 cases per million population and medium priority between 1,001-5,000 cases per million population.
Accordingly, the infection with these bacteria causes half to 1.5 years of disability in sufferers, per million population.
The list provides guidance on the development of new and necessary treatments to stop the spread of antimicrobial resistance (AMR ).
The Assistant Director-General of the WHO, responsible for antimicrobial resistance, Dr. Yukiko Nakatani, referring to the new list of resistant microbes and their impact on public health, noted the intensity of antimicrobial resistance, endangering the benefits of modern medicine and emphasized that the new list guides research and development investments for new antimicrobial drugs.
Accordingly, WHO Assistant Director-General for Universal Coverage and Communicable and Non-Communicable Diseases, Dr Jerome Salomon, pointed out that “Antimicrobial resistance compromises our ability to effectively address high-burden infections such as tuberculosis, leading in serious diseases and increased mortality rates”.
 Pseudomonas is a gram-negative bacterium and can transmit its resistance to drugs
Pseudomonas is a gram-negative bacterium and can transmit its resistance to drugs
The resistance is “sticky”
strong>
Critical priority pathogens include gram-negative bacteria that are resistant to last-line antibiotics as well as Mycobacterium tuberculosis that is resistant to the antibiotic rifampicin.
These microbes are major global threats due to their high burden and ability to resist treatment. But these microbes also have the ability to transmit resistance to other bacteria. Gram-negative bacteria have built-in abilities to find new ways to resist treatment and can pass genetic material that also allows other bacteria to become drug-resistant.
The changes
From the 2024 list (BPPL 2024), five pathogen-antibiotic combinations included in the 2017 list were removed, and four new combinations were added.
Enterobacteriaceae resistant to third-generation cephalosporins are included as a stand-alone element in the critical priority category underscoring the burden and the need for targeted interventions.
Carbapenem-resistant pseudomonas (CRPA) infection moved to high instead of critical priority category in BPPL 2024, reflecting the recent decline in resistance. Nevertheless, both investments in research and development of new antibiotics, as well as other strategies to prevent and control infection by resistant pseudomonas, remain important, due to the significant burden of the infection, which is observed in some areas.
< p>The 'difficult' microbes
The new WHO BPPL 2024 list includes the following bacteria, by category:
Critical priority
strong>
- Acinetobacter baumannii, resistant to carbapenems.
- Enterobacteria, resistant to third-generation cephalosporins and carbapenems
- Mycobacterium tuberculosis (Mycobacterium tuberculosis), resistant to rifampicin.
High priority
- Salmonella Typhi, resistant to fluoroquinolones
- Shigella (Shigella spp.), resistant to fluoroquinolones
- Enterococcus (Enterococcus faecium), resistant to vancomycin
- Pseudomonas aeruginosa, resistant to carbapenem
- Non-typhoidal Salmonella (Non-typhoidal Salmonella), resistant to fluoroquinolones
- Neisseria gonorrhoeae, resistant to third-generation cephalosporins or fluoroquinolones
- Staphylococcus aureus, resistant to methicillin
Medium priority
- Group A streptococci, resistant to macrolides
- Streptococcus pneumoniae, resistant to macrolides
- Haemophilus influenzae resistant to ampicillin
- Group B streptococci, resistant to penicillin.
source: in.gr